Useful Information on Common Cardiac Conditions
Chest pain is one of the commonest presenting symptom. It can be cardiac or non-cardiac. Analysis of the history and the characteristics of chest pain often give a clue whether it is cardiac. Investigations which are carried out to confirm chest pain due to coronary artery disease include ECG, exercise ECG, radionuclide myocardial perfusion scan, dobutamine stress echocardiogram, stress perfusion cardiac Magnetic Resonance Imaging scan, coronary CT angiogram and invasive diagnostic coronary angiogram.

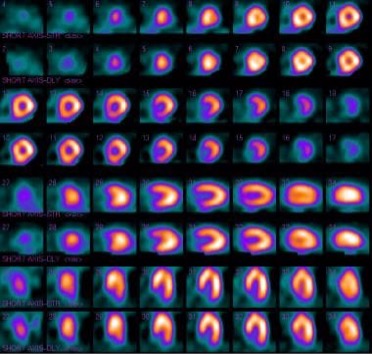
Radionuclide myocardial perfusion rest and stress images to look at areas of reduced perfusion caused by coronary artery disease.
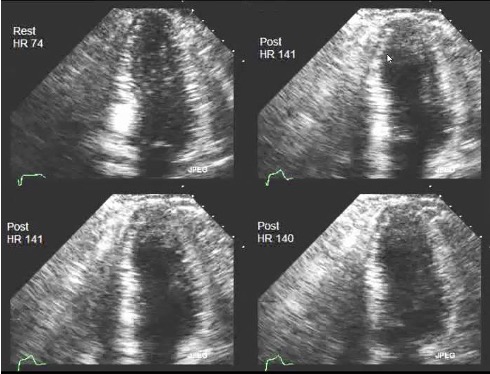
Stress echocardiogram with exercise or dobutamine to look regional wall motion abnormalities indicating obstructive coronary artery disease

Stress perfusion MRI looking at ischaemia and infarction.
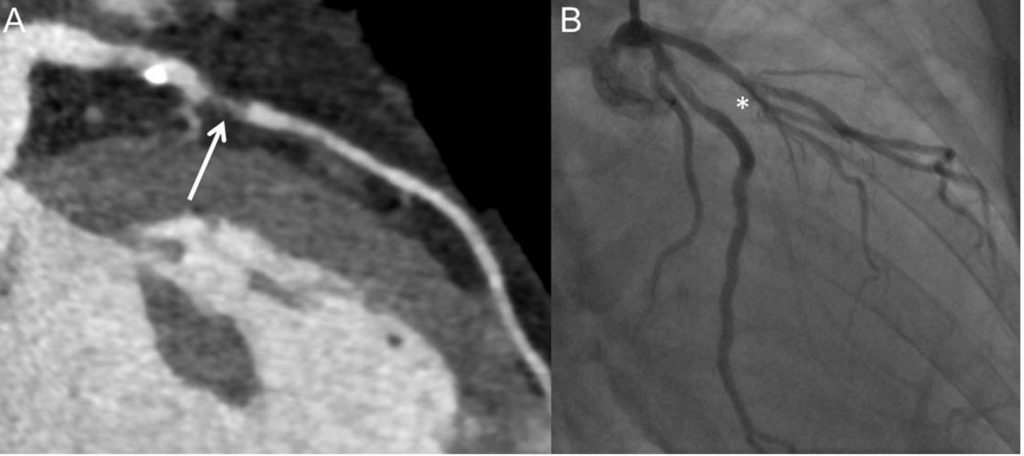
Resolution on Coronary CT angiogram (A) has improved greatly with ability to diagnose coronary obstruction compare with the gold standard invasive coronary angiography (B).
Palpitations are a reason for cardiology referral. These can be due to ectopic heart beats, atrial arrhythmias (abnormal heart rhythm arising from the upper chambers of the heart) or ventricular arrhythmias (abnormal heart rhythm from the lower chambers of the heart). By far, the most common type of palpitation is ectopic heart beats. This condition is usually not sinister, requiring reassurance only.
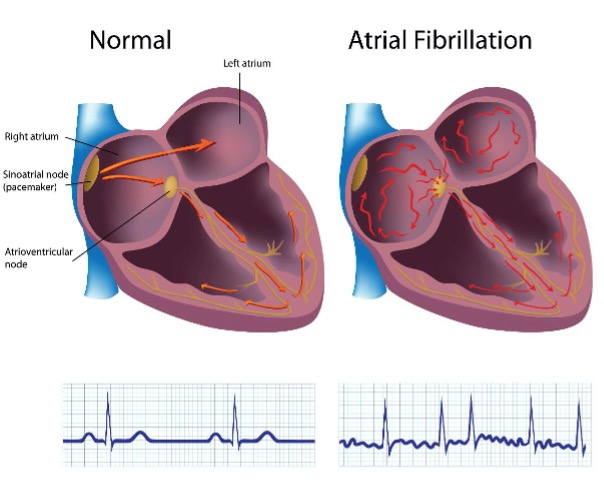
Atrial fibrillation is also a cause of palpitations and it is the most common heart arrhythmia. It arises due to abnormal uncoordinated fast electrical impulses from the atria (upper chambers of the heart) causing the heart to beat quickly. It can be short-lived and self-terminating known as paroxysmal atrial fibrillation or persistent, lasting for days and weeks often requiring electrical cardioversion or medication to restore regular rhythm. Atrial fibrillation can become permanent. It can cause symptoms of shortness of breath or chest pain due to the fast heart rate it causes. Some patients have no symptoms.
Atrial fibrillation increases the risk of developing blood clots within the left atrium (left upper chamber of the heart) which when dislodged can cause a stroke. About a fifth of strokes is due to atrial fibrillation. Some factors increase the risk of blood clot formation in atrial fibrillation including advancing age and the presence of such medical conditions as heart failure, high blood pressure, diabetes mellitus, previous strokes and vascular disease. Anticoagulant therapy with warfarin or direct oral anticoagulants (DOACs) is necessary for patients with an increased risk of stroke. Treatment of atrial fibrillation also involves the slowing of the heart rate using medication such as beta-blockers, calcium blockers and digoxin and restoring regular rhythm by means of electrical cardioversion or anti-arrhythmic medication in suitable patients. Following successful cardioversion, some patients may be considered for pulmonary vein isolation. These patients are usually symptomatic and continue to have bouts of atrial fibrillation despite receiving anti-arrhythmic medication. This procedure is complex often taking several hours using radiofrequency waves or cryoablation (freezing technique) to create thin lines of scar tissue to stop electrical impulses arising from the pulmonary veins (a known trigger of atrial fibrillation) from entering the heart. Further information can be obtained from dedicated websites like British Heart Foundation website.
Hypertension or high blood pressure is a common condition, occurring in a third to half the population after the age of 50 years. It is recorded in two numbers. The upper number is the systolic blood pressure and the lower one the diastolic blood pressure. Both readings are important. By definition, a clinic/office blood pressure of >140/90 is considered high. Such a reading is equivalent to an ambulatory blood pressure monitor or home blood pressure monitor average of >130/85. About 5% of hypertension is related to a secondary cause. Treatment is by means of lifestyle changes including reducing weight, regular exercise, reducing salt and alcohol intake. Medication used varies between countries. In the United Kingdom, the choice of medication is guided by age and race for maximum effectiveness. Combination therapy is usually necessary. Untreated hypertension can lead to heart attacks, strokes, heart failure, chronic kidney disease, hypertensive eye disease, peripheral vascular disease and vascular dementia. Treating blood pressure to a target of <120/80 can reduce the risk of heart attacks, strokes and death by 25%.
This is a condition caused by impaired contractility of the pumping chambers (ventricles) of the heart. The impairment can be either systolic or diastolic dysfunction. It causes symptoms of breathlessness, ankle or leg swelling and fatigue. Causes include previous heart attacks, idiopathic dilated cardiomyopathy (no obvious cause), familial/genetic cardiomyopathies, untreated high blood pressure, alcoholic cardiomyopathy, severe heart valve disease, tachycardia-related cardiomyopathy (due to prolonged fast heart rate like in uncontrolled atrial fibrillation) and chemotherapy-related cardiomyopathy. Investigations carried out include BNP blood tests, echocardiograms, cardiac MRI, cardiopulmonary exercise tests (CPEx) and cardiac catheterisation. Treatment involves treating the cause of heart failure, diuretics, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers, mineralocorticoid receptor antagonists (eplerenone and spironolactone), angiotensin receptor neprilysin inhibitor (ARNI – sacubitril/valsartan) and certain SGLT2 inhibitors (dapagliflozin and empagliflozin). Certain patients may benefit from specialised pacemaker and implantable cardioverter defibrillator device therapy.

Aortic stenosis is the most common heart valve disorder in the developed world. The aortic valve is the valve which separates the main pumping chamber of the heart (left ventricle) and the aorta. It can become degenerative and thickened with age, causing the valve to narrow thus impeding blood flow. The condition can be suspected by using the stethoscope and feeling for the characteristics of the pulse. An echocardiogram is used to assess the severity. When severe, it causes chest pain, shortness of breath and fainting. If untreated, it reduces survival significantly and when critical, it can cause sudden fatality. Treating is by means of surgical aortic valve replacement (open heart surgery) or transcatheter aortic valve implantation (TAVI), the latter is a catheter-based procedure usually using the femoral artery approach from the groin for patients who are too frail to have major open heart surgery. TAVI is increasingly used for patients with low surgical risk but the durability of the TAVI valve especially in the younger patients needs further evaluation.
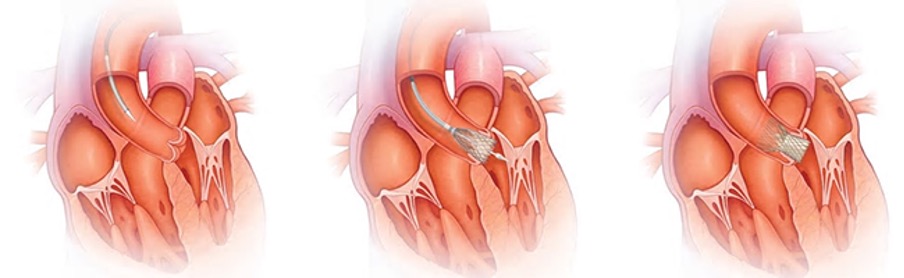
TAVI Procedure
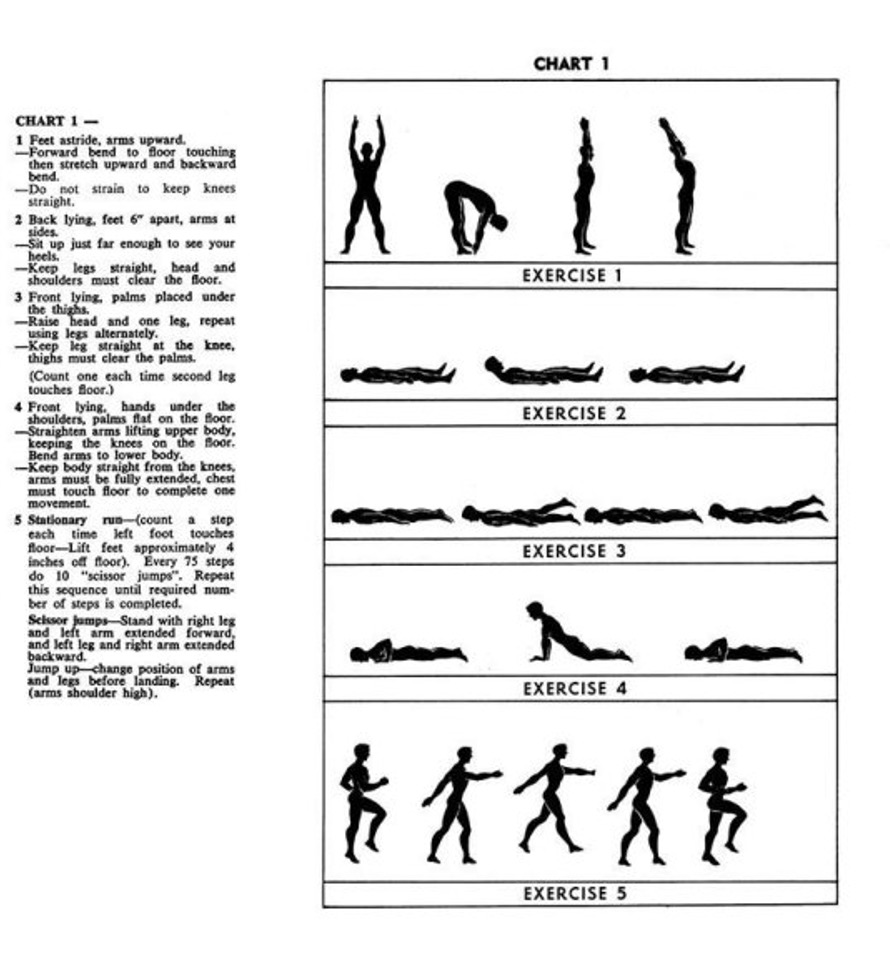
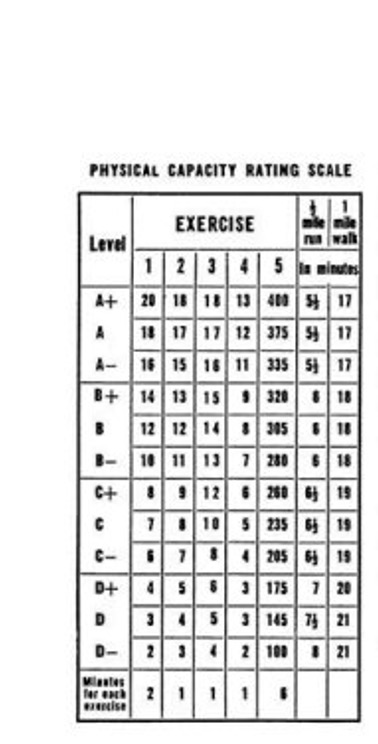
Physical training is generally good for the heart with some exceptions. The 5-BX exercise protocol has been adopted for cardiac rehabilitation in heart failure patients. An adapted training schedule is given below.